‘Last Mile Healers’ use solar clinics to close Africa’s health access gap
By Brian Ochieng Akoko, Reporter | Nakuru City – Kenya.
Access to healthcare remains one of Africa’s most persistent development challenges. Millions of people live in remote, rural areas. They are cut off from centralized hospitals and clinics by vast distances and poor infrastructure.
This access gap is often fatal. Simple, treatable conditions become life-threatening emergencies. Infant mortality rates remain high. Preventable diseases spread rapidly. Maternal health outcomes are critically poor.
The solution is not always to build more large hospitals. The solution is often to rethink delivery. The medical services must go to the people. The people cannot always come to the services.
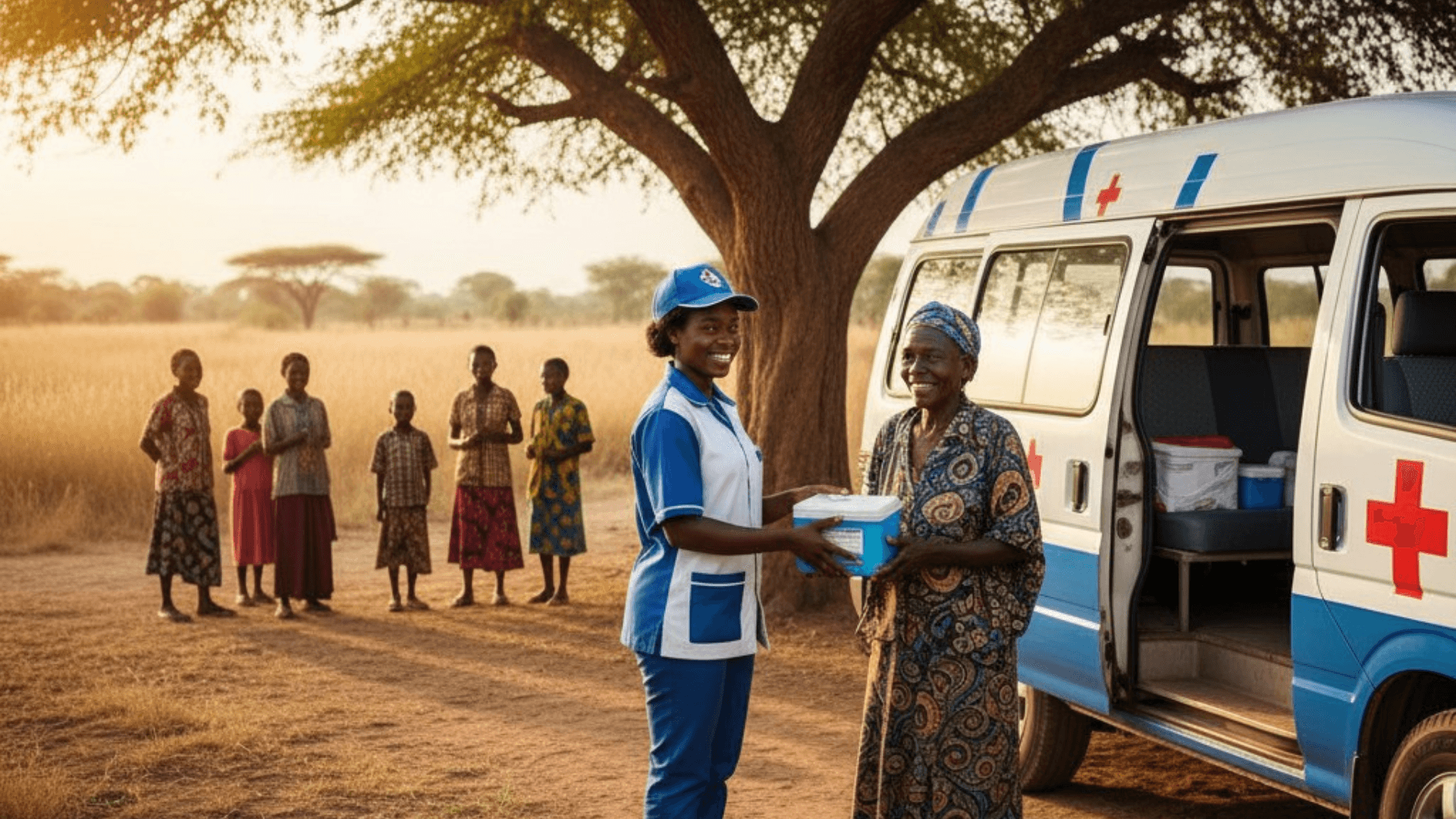
This shift is powered by two vital forces: mobile clinics and Community Health Workers (CHWs). These individuals and units are the Last Mile Healers. They are closing the gap between central care and isolated populations.
They use decentralized models and simple technology. They deliver essential, life-saving care directly to the village gate. This approach is proving to be cost-effective. It is also culturally appropriate and highly sustainable.
The Power of the Community Health Worker

The Community Health Worker (CHW) is the bedrock of this decentralized model. CHWs are local residents. They are trained in basic health procedures. They are the trusted link between the formal health system and the community.
Their training is focused on primary care and prevention. This includes maternal and child health. They manage common illnesses like malaria and diarrhea. Crucially, they track vaccination schedules.
They ensure children receive essential immunizations. They are equipped with basic diagnostic tools and mobile technology. This allows them to record patient data instantly. They can send critical alerts to supervising nurses or doctors in distant clinics.
The CHW model is effective because it is built on trust and cultural knowledge. A CHW speaks the local language. They understand the community’s customs. They are a familiar and accepted figure.
This is essential for sensitive health issues, such as reproductive health or mental well-being. The CHW provides a vital counter-narrative to traditional stigma and misinformation.
They provide education and reliable medical advice. This local presence drastically improves health-seeking behaviour. It encourages early intervention before conditions become critical.
Mobile Clinics: Bringing the Hospital to the Village
Complementing the CHWs are the innovative mobile clinics. These are often repurposed vans or trucks. They are equipped with advanced diagnostic tools, consultation rooms, and sometimes even dental units.
Many are now powered by solar panels. This makes them fully autonomous. They can operate in areas without electricity. Mobile clinics run on a carefully planned schedule. They visit remote villages that have no permanent clinic.
They provide services that are too complex for a CHW. This includes complex prenatal check-ups, minor surgeries, and specialized diagnostics. The logistical challenge is immense.
It requires careful coordination of staff, medicines, and equipment. However, the impact is undeniable. A mobile clinic can deliver a full suite of services to hundreds of people in a single visit.
This significantly reduces the need for patients to travel vast distances. It saves them time and money. For chronic diseases like diabetes or hypertension, mobile clinics provide the necessary follow-up care.
They ensure patients adhere to their treatment plans. This decentralized delivery model is key to strengthening the health system’s ability to reach everyone, regardless of geography.
Digital Health and Data Management
The final piece of the puzzle is digital health. Simple mobile apps are revolutionizing data collection. CHWs use tablets or smartphones to record patient information in real-time.
This data is then aggregated and analyzed by central health departments. This provides an accurate, up-to-the-minute picture of community health. It allows health officials to quickly identify disease outbreaks. They can track vaccination coverage.
They can allocate resources where they are most needed. This data-driven approach is transforming health management. It moves from reactive crisis management to proactive, preventative care.
Digital tools also provide decision support for CHWs. They guide them through diagnostic protocols. They ensure accurate treatment. This combination of human trust, mobile infrastructure, and digital data is a powerful force.
The Last Mile Healers are demonstrating that effective healthcare is not about proximity to a capital city. It is about dedication, innovation, and reaching every single person.


Daj svoj stav!
Još nema komentara. Napiši prvi.